Genetics and its relationship with fertility
It is estimated that 25% of women will suffer an abortion in their lifetimes. 50% of these miscarriages involve some type of chromosomal alteration. These abnormalities are often related to advanced maternal age.
There are also many genetic diseases. It is estimated that 3-4% of births will suffer from such a disease. According to the Spanish Federation of Rare Diseases, there are between 5,000 and 7,000 rare diseases. 80% of these are of genetic origin and, therefore, susceptible to being transmitted to our children.
Both scenarios pose a major challenge to assisted reproduction. Detecting these disorders early allows us to achieve high rates of healthy new-borns at home.
High complexity reproductive genetics unit
The Equipo Juana Crespo Genetic Unit provides personalised strategies for patients, offering a wide range of genetic studies according to their reproductive stage, family history and past pregnancy loss(es).
This unit’s primary goals are:
- Personalised genetic counselling consultation. For each case, it is important to know the family genetic history and consider the best reproductive options to achieve a healthy pregnancy.
- Proper advice on the appropriate tests to be performed at each stage.
Genetic testing in pregnancy planning
Genetic testing at the preimplantation stage of the embryo
PGT or Preimplantation genetic testing. The study performed on embryos generated through in vitro fertilization techniques, which reveals whether they are affected by any chromosomal or genetic alteration before transfer to the mother’s uterus. This prevents the transfer of embryos that may cause serious diseases or that might not result in a healthy or full-term pregnancy.
Depending on the study objective, the types of PGT are:
Prenatal or pregnancy stage Genetic Testing
Frequently Asked Questions
First, we must be aware that hereditary diseases are caused by a series of changes, also called mutations, in the genes making up our DNA. We have two copies of most genes, one inherited from our mother and the other from our father.
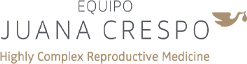
The number of healthy embryos expected depends on the type of inheritance of these changes.
If, for example, the disease has an autosomal dominant inheritance, 50% of the embryos generated are likely to be healthy and transferable. Only half of the children will inherit the mutation from the affected parent.
However, if the disease is autosomal recessive, it will only manifest itself if both copies of the gene are affected, i.e., the mutation has been inherited from both parents. If this occurs, the probability of an affected child in each pregnancy is 25%. If only one parent has a disease-causing variant, their children will not be affected, and will have a 50% chance of being healthy carriers like their parent.
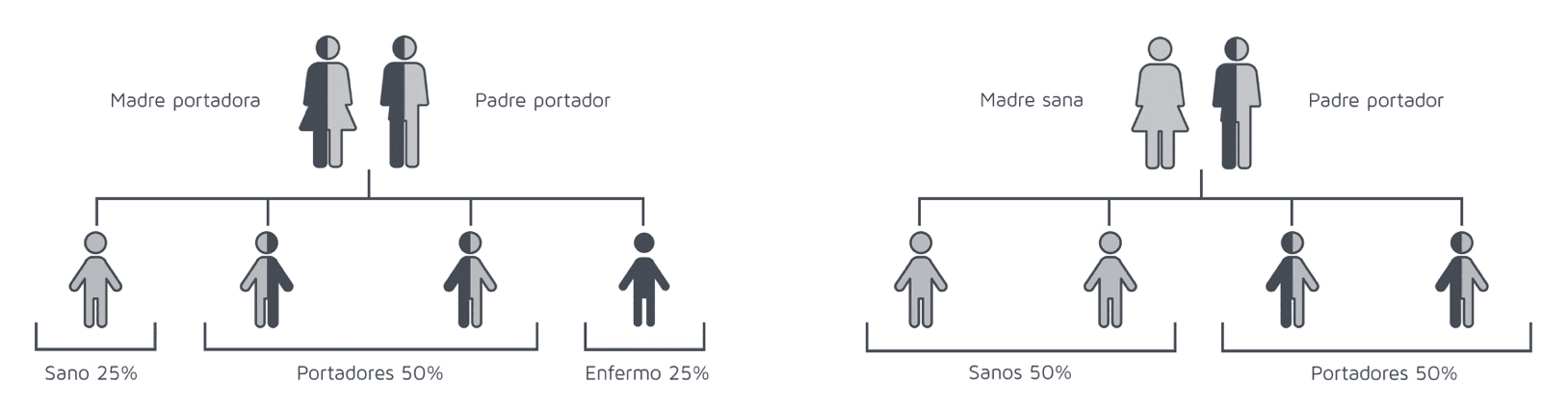
There are also diseases with a particular type of inheritance. When the disease-causing variants are in the X chromosome, they are called X-linked. Females have two X chromosomes while males have only one. Males who inherit these variants are always affected, while females are often unaffected carriers.
PGT and TGP refer to the same term, but in English and Spanish respectively. In English, PGT stands for Preimplantational Genetic Testing. As it’s the international scientific language, this is the most common. TGP in Spanish refers to the same test. PGD stands for Preimplantational Genetic Diagnosis and PD for Preimplantational Diagnosis. The latter two are increasingly uncommon, as this analysis is not considered a diagnosis as such, but instead screening of a representative part of the whole embryo.
It may seem like the PGT-A would guarantee success for all patients if a healthy embryo is transferred. However, this is not the case. If there is no clear indication, embryo biopsy is not recommended because, after all, it is an invasive technique. This technique has been proven to reduce implantation failures and miscarriages, but at EMC we prefer to personalise all treatments and techniques, including PGT.
PGT-A does not study all existing diseases. It studies chromosomal alterations, some of which may give rise to diseases we are already aware of, such as Down syndrome, Edwards’ syndrome, Patau’s syndrome, etc. Although science is advancing rapidly and the panel of genes to be studied is becoming broader, there is currently no test that guarantees a completely healthy child with no diseases.
The following results can be obtained from a PGT-A study:
- Normal embryo: All cells analysed have the correct number of chromosomes and are therefore suitable for transfer.
- Abnormal embryo: The alteration of one or more chromosomes is observed in all the cells analysed. For example, an extra chromosome 18 (trisomy) is responsible for Edwards’ syndrome. This embryo is not suitable for transfer.
- Potential mosaic embryo: Both altered and normal cells are observed in the set of cells analysed. Depending on the characteristics of the anomalies involved, a recommendation may be made regarding considering it for transfer. This should be discussed in a genetic counselling consultation with qualified personnel.
Given maternal age is a determining factor in the number of normal embryos, it should be known that the older the patient, the lower the probability of getting a normal embryo to transfer.
However, the probability of obtaining potential mosaic embryos is independent of maternal age. At EMC, our potential mosaic embryo rate is around 12%.
Personalised counselling is recommended in each case to indicate non-invasive prenatal testing (NIPT). However, it is important to know that no modern genetic test is 100% diagnostic. Therefore, even if a PGT-A is performed, a NIPT may still be done later.
Non-invasive prenatal testing does NOT study hereditary diseases. This testing only studies chromosomal alterations. If there is a suspicion of a pregnancy affected by a hereditary (monogenic) disease, invasive prenatal testing on an amniotic fluid sample (amniocentesis) is indicated.
When transferring an embryo analysed via PGT-M, the recommendation is the same, but the probability of an altered result is considerably lower.