The success in pregnancy rates through assisted reproduction techniques depends on different factors, including uterine functionality or embryonic quality. In order to determine these factors it is necessary to do an embryo grading.
Many studies related to embryonic quality, have been collected and analyzed over time in order to create a standardized guide to morphological and kinetic patterns of the embryos.
This guide will allow us to understand what embryo grading consists of based on the embryos development, which is directly related to their potential for implantation.
On the other hand, there are many patients who trust our embryologists to take care of their eggs and embryos. And it is perfectly normal for you to be concerned about the conditions in which we maintain and care for them. This is why we are going to tell you how the stay of the gametes develops in our in vitro fertilization laboratory.
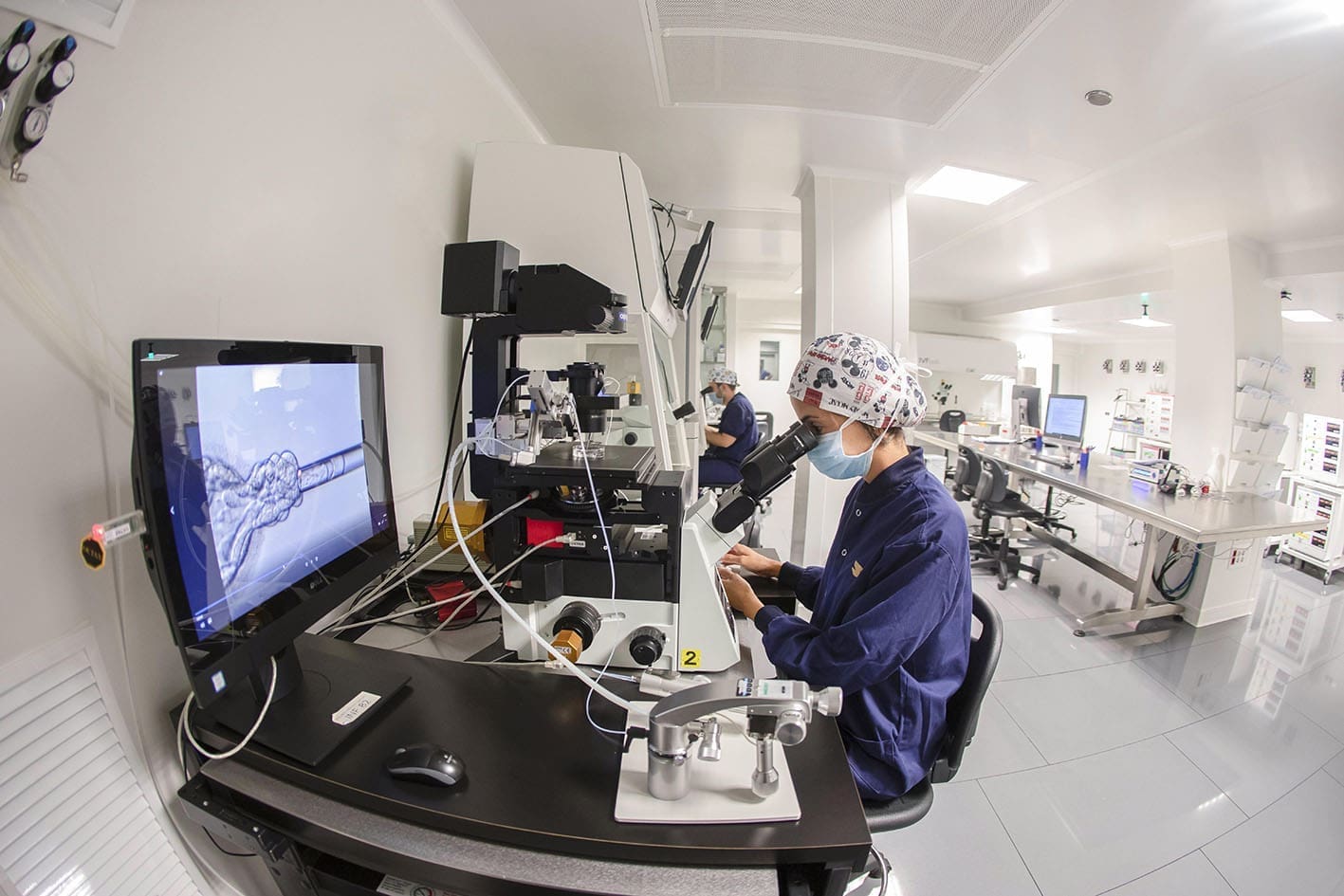
HOW IS OUR FIV LABORATORY?
First of all, we must clarify that our laboratory is a “clean room”. This means that it is a space specifically designed to maintain certain environmental parameters. To do this, we have an advanced security system that allows us to have strict control over the levels of humidity, lighting, temperature, pressure, etc.
This allows us to prevent any external agent contaminating or interfering with the embryo culture. This way, we can always keep the samples in the ideal environmental conditions.
In addition, the laboratory has a rank of maximum quality, granted to us due to the accomplishment of different norms of excellence like: the norm ISO 9001 and the UNE 179007 (this last one is specific for laboratories of assisted reproduction). These certificates guarantee our patients that the laboratory exceeds the maximum quality standards.
In addition, to ensure the excellent conditions, every day and in parallel, an exhaustive protocol is done where each of the quality parameters are reviewed. This way, we will ensure that optimal environmental conditions for our embryonic cultures are met at all times, since the success of the treatment will depend on it.
THE BEGINNING OF EMBRYONIC CULTURE
Embryo culture begins right at the moment of the follicular puncture, the moment we would consider day 0. In this instant, one of our embryologists collects the oocytes and begins to prepare them for, a few hours later, doing the in vitro fertilization (this will be done either by classic in vitro fertilization or by Intracytoplasmic Sperm Injection -ICSI-). At this point, our experts will observe how the gametes are morphologically and whether or not they show any relevant alteration.
MAINTENANCE OF THE GAMETES IN THE IVF LABORATORY
From the moment of the follicular puncture and throughout the period of embryonic evolution, the oocytes and subsequent embryos will be arranged in culture plates. These are containers especially designed to provide the specific nutrients at each stage, necessary for the viability of the cell, and to protect them from the external environment.
These plates will be kept in incubators, under a particular atmosphere of gases and temperature, which seek to emulate the natural environment of embryonic development.
It is worth mentioning that, in our laboratory, each patient has their own exclusive incubator during the whole embryonic development. With this, we seek to minimally reduce the alteration of the atmosphere under which the embryos are located and, furthermore, to provide additional security regarding the traceability of each patient’s plates.
The particular conditions of these incubators, such as temperature, pH of the culture medium or the concentration of available gases (O2 and CO2), are continuously analyzed during the course of the embryonic development in order to verify the quality of the conditions.
Additionally, all equipment is monitored by continuous recording systems that verify that the ideal conditions have not suffered variations that damage the atmosphere.
FIRST PHASE OF EMBRYONIC DEVELOPMENT
On day +1, that is, the day after the follicular puncture and the in vitro fertilization, the zygotes are evaluated to see which have been fertilized. To do this, our embryologists will observe the presence of a series of indicative asigns and those whose fertilization has been correct will be selected.
On this day +1, except in specific cases where characteristics linked to poor embryonic development are observed (number of nuclear precursors or vacuoles), we cannot classify the embryos based on reliable quality criteria.
EMBRYO GRADING
On days +2 and +3, the zygote has begun to divide and it goes on to form a cell stage embryo. It is then that it begins to be catalogued according to its morphokinetic characteristics: based on the number of cells it has, symmetry, fragmentation degree or number of nuclei, among others.
To classify the embryos in this phase and thereafter, we use the guidelines established by the Association for the Study of Biology of Reproduction (ASEBIR). Based on this guide, we provide each embryo with an alphabetical quality A, B, C or D, being A the best possible quality.
This classification, being the most extended among the Spanish reproductive community, allows us to unify criteria with the rest of fertility clinics and to extrapolate the global data of our cycles. This way, we will be able to carry out statistical and comparative studies with the rest of the assisted reproduction centers.
The grading seeks to discern between embryos with high implantation potential and those with low implantation potential.
On day +3 the embryonic genome is activated, so overcoming this barrier is crucial for the embryo’s destiny. But it will not be until day +4, when the embryo will finally form a structure with very compacted cells, something we call a morula.

THE BLASTOCYST STAGE
The last embryonic stage we can reach in the laboratory is the blastocyst stage. This stage is reached on day +5 and +6 of embryonic development although, in very particular cases, the culture could be prolonged until day +7.
The blastocyst is characterized by a central cavity (blastocele) and two different cellular regions: the trophoectoderm (precursor of the placenta and extra-embryonic tissues) and the internal cell mass (MCI; precursor of the embryonic tissue).
To grade them, we also use the guidelines established by ASEBIR. At this stage the grading is made based on the two existing cellular regions. An alphabetical letter (A, B, C or D) is given to the trophoectoderm and another to the ICM.
Once the embryonic cohort has been evaluated and the qualities classified, an order of the embryos in the cohort is established. Thus, we classify them from the best of them to the worst, also taking into account the evolution they have had throughout the culture.
WHAT HAPPENS TO LOWER QUALITY EMBRYOS?
It should be noted that the embryos with embryonic quality D and those that are not viable are directly discarded because they lack (almost or completely) the potential for implantation.
Based on the classification of embryos that we have explained, our embryologists organize the embryos to be transferred, vitrified, or to be biopsied, in order of quality.
Determining the correct elective order of the embryos is crucial, since the success of the reproductive cycle will depend on the implantation potential of the chosen embryo. For this reason, we make an exhaustive analysis of all the stages of the evolution of each embryo in our laboratory, collecting any parameter that can determine if one evolutionary embryo could have a greater or lower potential for implantation than another (even if it shows the same quality in the blastocyst stage).
It is worth mentioning that the embryo culture can be short (ending in D+3, when the embryos are transferred or vitrified in the cell stage) or long (ending in day +5, +6 or +7, when the embryo reaches the blastocyst stage) and will always depend on the particular case of each patient.
HOW IS THE EMBRYO SELECTION DONE IN JUANA CRESPO TEAM?
The decision to choose one type of culture over the other is agreed upon by the medical team and the laboratory team.
When the cycle of assisted reproduction of our patient is designed, some premises are established. However, these will be evaluated and reviewed time and again throughout the embryonic evolution, always seeking a completely individualized and specialized treatment for each specific case.
If you are interested in finding out about your fertility or receiving more information about this subject, please do not hesitate to contact us. Equipo Juana Crespo is happy to receive you in one of our clinics to offer you the advice you need.